Journal of Medicine, Engineering, Environmental and Physical Sciences (JOMEEPS), Vol. 2, No. 1, March 2024. https://klamidas.com/jomeeps-v2n1-2024-01/ |
||||||||||||||
|
Influence of Ward Spatial Features on Staff Activities of Healthcare Delivery in Public Tertiary Mental Health Facilities in Southeast Nigeria C. C. Onwuzuligbo
ABSTRACT Cognitive psychologists have advanced the argument that the configuration of spaces is instrumental in patterning the movement and activities, as well as modifying the functions, of persons using such spaces. The objective of the study was to examine the relationship between type of ward layout (which is a variable of ward spatial features) and staff activities of healthcare delivery in public tertiary mental healthcare facilities which offer inpatient psychiatric services in Southeast Nigeria. Out of the 302 staff who make ward contact with the patients, 190 were sampled for this cross-sectional study. Statistical analysis was carried out using frequency distribution, descriptive summary measures, and Point-Biserial correlation (α = 0.05) using SPSS-20. Data on the following were collected using structured questionnaires: demographic characteristics of the health workers (gender, years of experience in MHC delivery, and designation); specific ward features (social density, type of ward layout, location of nursing station, type of ward supplies service); and the extent to which staff agree to the influence of each of these ward features on planned patient contact, structured patient observation, and quick response to patient. It was established that type of ward layout does not significantly correlate with overall staff activities. even though the influences of the individual ward features correlated significantly. Inconsistent findings with previous studies may be influenced by the differing socio-cultural context within which the study was carried out and ill-conceived notion about mental health, thus, preventing patient-centred model of care in psychiatric hospitals in the study area. Recommendations include use of private rooms and cubicle wards for patients with decentralized nursing stations, and mental health literacy for care givers on aspects of patient-centred model of care. Keywords: direct patient care, hospital affordance, staff activities, ward spatial feature
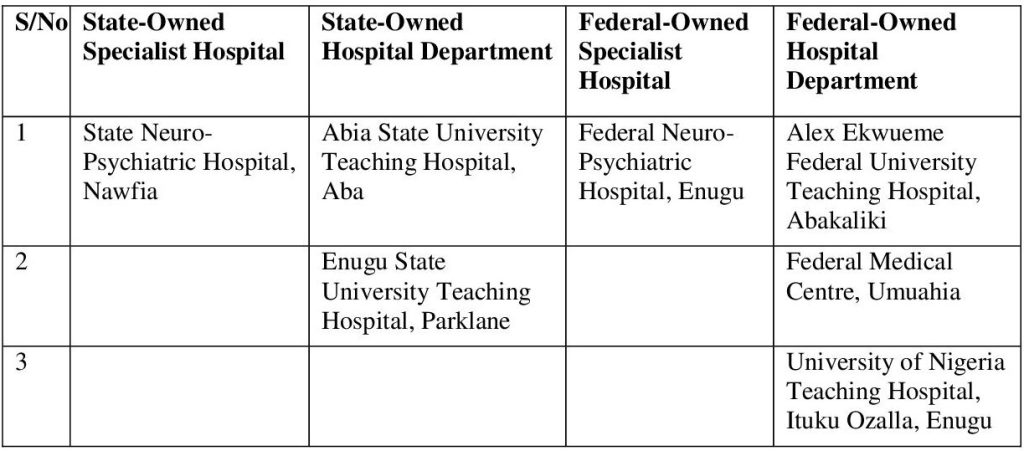
INTRODUCTION Technological advancements have improved the efficiency of staff activities in healthcare settings. However, concerns have been raised on the use of architectural design of the physical environment in these settings to facilitate staff functions, patient safety and other patient outcomes (Reiling et al., 2008). Cognitive psychologists have advanced the argument that the configuration of spaces is instrumental in patterning the movement and activities, and modifying the functions, of persons using such spaces (Reiling et al., 2008) for improved efficiency in executing functions. To address the challenge of efficiency in carrying out functions, intrinsic adjustments to organizational climate, healthcare protocols and the physical settings of wards are necessary, and need to align so that the caregivers and the resources that support them are set up for proper patient care (Tyson et al., 2002; Ulrich,2006, Ulrich et al., 2004). Several studies have associated design features of wards with positive patient outcomes such as reduced anxiety, higher levels of satisfaction with care, reduced aggression (need for restraint and seclusion), improved social interaction with fellow patients and staff, increased compliance with treatment plans, reduced depression and stereotypy (Stolz et al., 2015; Lockman et al., 2017; Ulrich et al., 2014; Bressington et al., 2019; Grootens-Wiegers et al., 2018; Holohan & Saegert 1973). However, Tyson et al. (2002) noted that the positive modification in behaviour observed in patients may not entirely be in response to changes in ward features alone. They may be more attributable to changes in staff work activities and behaviours as well as changes in organizational milieu (indirect influences) than the change in itself (direct influence). It is, therefore, imperative to examine what influence ward spatial features have on staff activities, such that they carry out these activities effectively, thereby enhancing the therapeutic milieu of the ward. Having seen the likely influence of staff work activities on patient outcome, it is surprising only a few studies have been done in that regard (Lauder et al., 2006; Stuart et al., 2015). The majority of these were focused on regions representative of high income countries. It is therefore imperative to carry out similar studies in low-and-middle income countries such as Nigeria, considering that low-and-middle income countries generally do not have comprehensive mental healthcare policies; where they do exist, they are ineffectively implemented due to shortage of resources such as infrastructure, personnel and funding (Gureje & Alem, 2000; Gureje et al., 2005; Thornicroft et al., 2017). It is for this reason that this study aims to assess the influence of ward spatial features on staff activities of healthcare delivery in public tertiary mental health facilities in southeast Nigeria, with a view to proffering design modifications to ward design for improved staff functions. The current investigation is part of a wider study that assesses the effects of the physical environment on mental healthcare delivery in public mental healthcare facilities in Southeast Nigeria with the aim of generating design strategies that would significantly improve healthcare delivery outcomes for both staff and patients. As a specific objective, the current study seeks to examine the relationship between type of ward layout (which is a variable of ward spatial features) and staff activities in healthcare delivery. The null hypothesis postulated for this unit of investigation is ‘There is no significant relationship between type of ward layout and staff activities of healthcare delivery in the study area.’ METHOD The research area is the South-East geo-political zone of Nigeria comprising five states namely: Abia, Anambra, Enugu, Imo and Ebonyi States. Southeast Nigeria is located within latitudes 4°4’35” N and 7°7’44” N of the Equator, and longitudes 7°54’26” E and 8°27’10” E of the Greenwich Meridian. According to the 2006 population census conducted in Nigeria, southeast Nigeria has a population of 16,395,555 persons (Federal Republic of Nigeria Official Gazette, 2009). This cross-sectional study was conducted in the public tertiary health facilities of the region which offer inpatient mental health services. Seven operational facilities were identified, each falling under any one of the following category: state-owned specialist hospital, state-owned hospital department, federal-owned specialist hospital, federal-owned hospital department. See Table 1. Table 1: Stratification of Public Inpatient Mental Healthcare Facilities in Southeast Nigeria by Ownership-Specialty
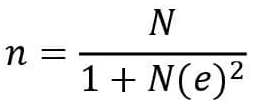
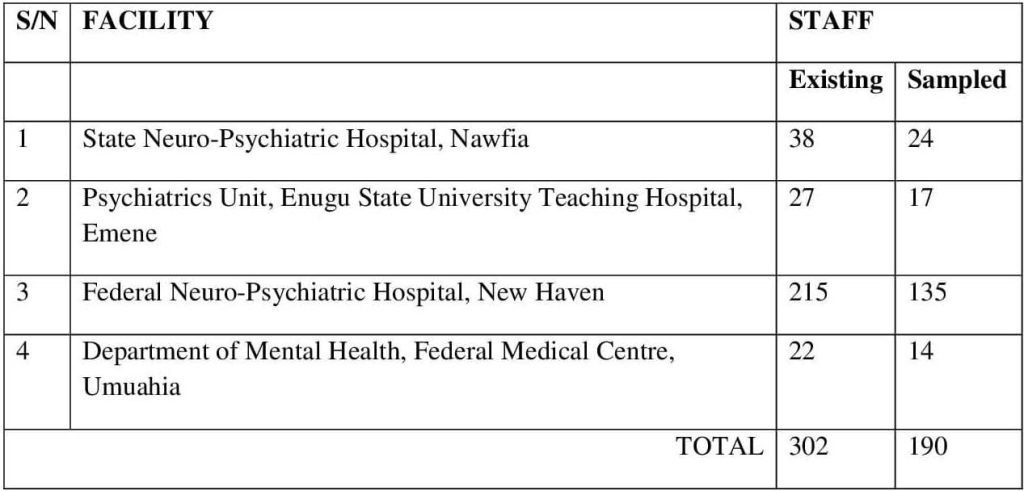
Following this stratification, random sampling by balloting was applied to each stratum (having more than one facility) to identify the facility to be surveyed. The following were selected: i. State-owned specialist hospital: State Neuro-Psychiatric Hospital, Nawfia, Anambra state (SNH) ii. State-owned hospital department: Psychiatrics Department of Enugu State University Teaching Hospital, Parklane (ESUTH) iii. Federal-owned specialist hospital: Federal Neuro-Psychiatric Hospital, New Haven (FNH) iv. Federal-owned hospital department: Department of Mental Health of Federal Medical Centre, Umuahia, Abia State (FMC) The number of mental healthcare (MHC) workers for each facility was obtained from the nominal roll of staff for each facility. The respondent sample size was derived using the Taro Yamane formula (Israel, 2012) at 95% confidence level and maximum degree of variability of ρ =0.05, and adjusted for non-response rate of 10%:
Where: n= Sample size for finite population N= Population size = 302 e= level of precision = .05 The obtained figure (138 staff) was distributed among the sampled facilities according to the ratio each contributes to N, and the research tool shared accordingly (Table 2). Table 2: Respondents sample size in sampled facilities
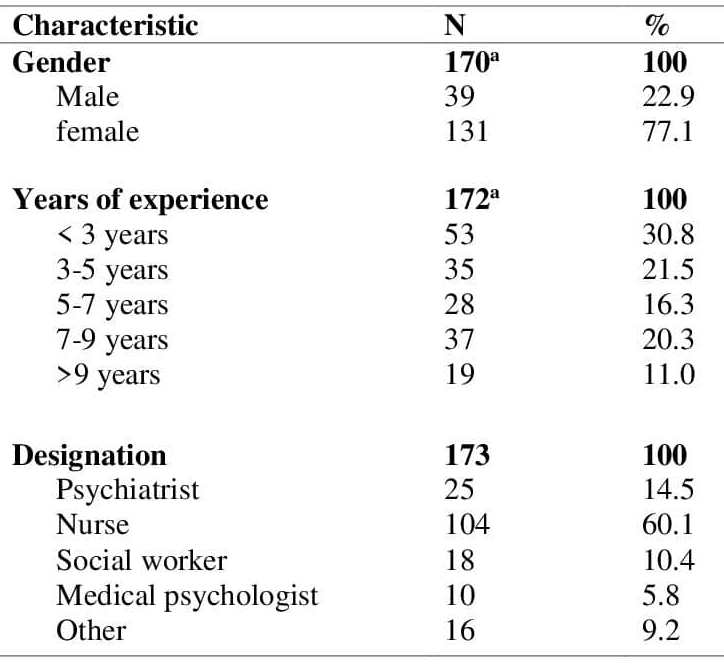
The research tool was designed to elicit data on the demographic characteristics of the health workers (gender, years of experience in MHC delivery, and designation); specific ward features (social density, type of ward layout, location of nursing station, type of ward supplies service); and the extent to which they agree to the influence of each of these ward features on planned patient contact (patient handling), structured patient observation, and quick response to patient. These were ranked on a 5-point Likert scale. The research tool was subjected to the scrutiny of experts in the specialties of Architecture, Psychiatry, Psychology and Statistics to ensure content validity while test-retest reliability method was adopted to ensure reliability of the tool. The study protocol was approved by the Research and Ethics Committees of the individual health facilities after which the questionnaires were distributed to consenting health workers. Participants also reserved the right to withdraw from the study if and when they so wished, and were under no obligation to return questionnaires upon completion. Data collection across the 4 facilities was carried out within 6 months (June to November, 2022). Statistical analysis was done with Statistical Package for Social Sciences (SPSS-20) using descriptive summary measures and frequency distribution, Point-Biserial Correlation analysis. RESULTS Of the 190 questionnaires distributed, 173 were returned, representing 91.1% response rate. The total number of valid responses per variable of interest was indicated. Table 3 describes the socio-demographic characteristics of the study population. Data collected on gender of staff show that more female staff (77.1%) work in the study area while 22.9% were identified as males. A greater percentage of staff had less than 3 years of experience (30.8%), closely followed by staff with 3-5 years of experience (21.5%). Staff with over 9 years of working experience were least represented (11%). More than half (60.1%) were nurses, 14.5% were psychiatrists, 10.4% were social workers while 5.8% were medical psychologists. 9.2% indicated to be working in other capacities not captured. Table 3: Socio-demographic characteristics of participants
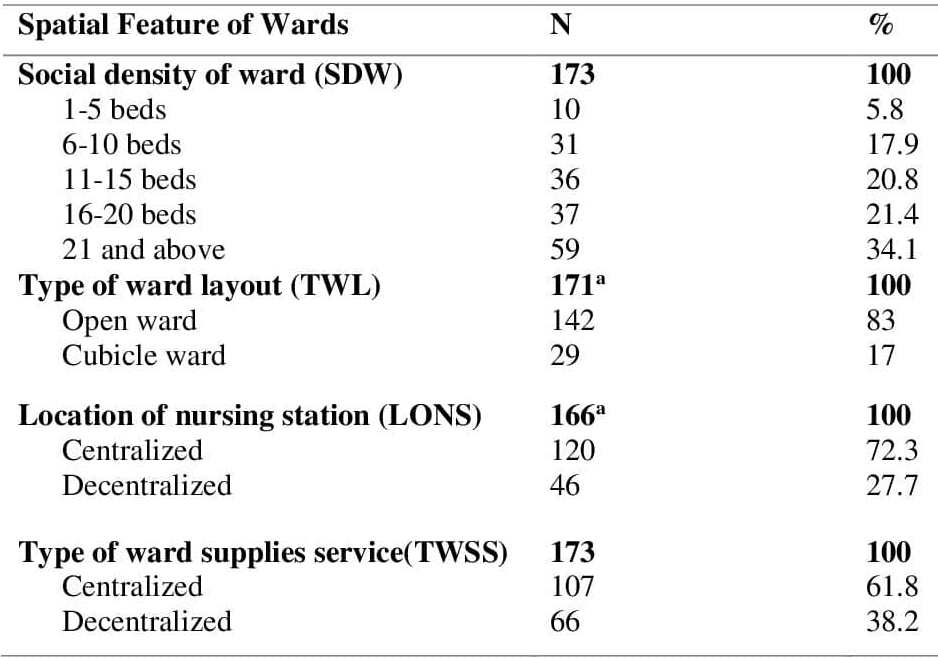
aFigures do not add up to 173 due to missing data. Table 4 shows the distribution of ward features among staff in the study area. With respect to social density of ward, results show that 94.2% of staff work in high multiple-occupancy wards. More specifically, 34.1% work in wards of at least 21 beds per ward, 21.4% work in 16-20 bed-wards, 20.8% work in wards with between 11 and 15 beds, 17.9% work in wards with 6 to 10 beds, while less than 5.8% work in wards with less than 6 beds. In terms of type of ward, 83% reported to be working in open wards while 17% reported to be working in cubicle wards. While 72.3% work in wards with centralized nursing station, 27.7% work from decentralized nursing stations. As far as type of supplies service is concerned, 61.8% reported to be working in wards with centralized supplies service while 38.2% operate with decentralized ward supplies service. Table 4: Distribution of spatial features of wards
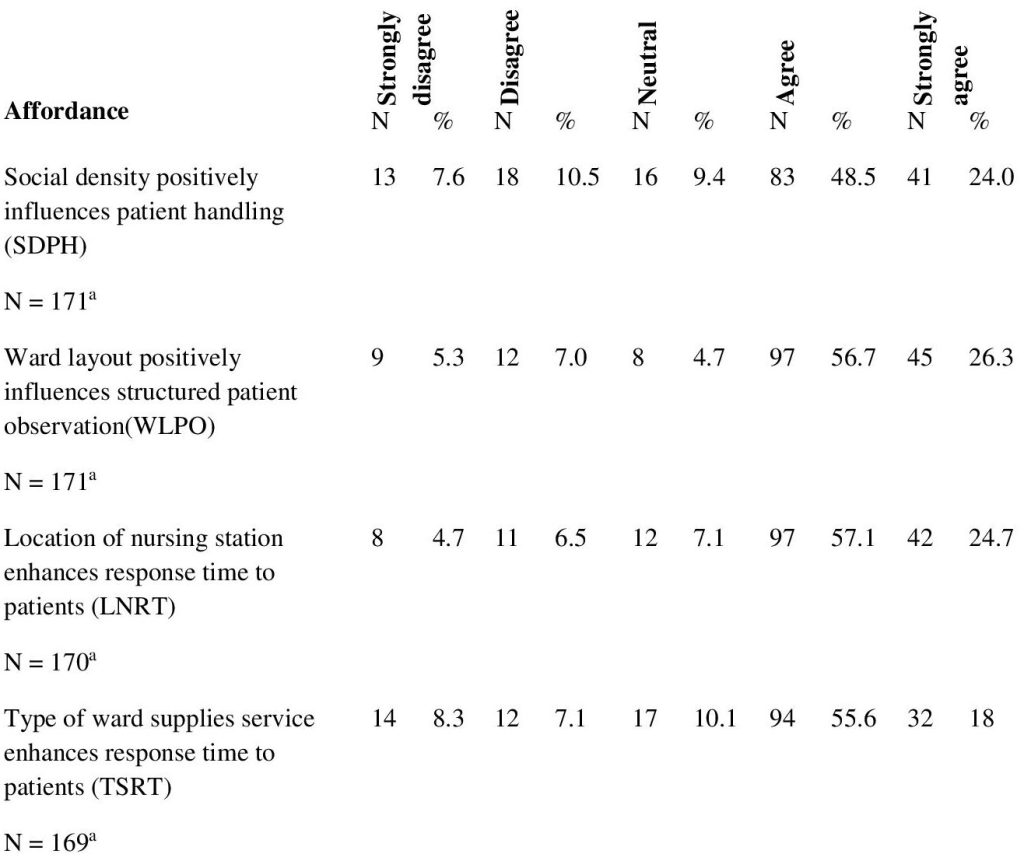
aFigures do not add up to 173 due to missing data. Table 5 shows the extents to they agree to the influence of specific ward features as identified in Table 4. A greater majority of staff (72.5%) in the study area agree to varying extents that the social density of the ward in which they work positively influences how they handle patients. To this statement still, 18.1% disagreed to different degrees. On the influence of ward layout, 56.7% and 26.3% respectively agree and strongly agree that the layout of wards in which they work enhance visibility to patients. On the other hand, 7% and 5.3% respectively disagree and strongly disagree to this. When queried on response time to patients, 57.1% and 24.7% respectively agree and strongly agree that the location of nursing station from which they operate was instrumental in responding quickly to patients in the event of reactive patient contact. However, a minority of 11.2% disagreed/ strongly disagreed to this assertion. Again, more than half of the staff (73.6%) affirmed, to varying extents, that the type of ward supplies services enhanced response time to patients while 15.4% of staff disagreed to varying extents to this statement. Table 5: Ratings of influence of spatial features of wards
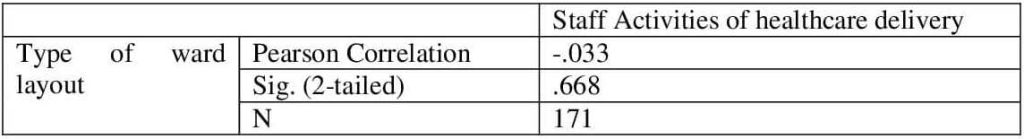
aFigures do not add up to 173 due to missing data. The variable ‘type of ward layout’ (TWL) was used as the dependent variable because it is key in defining spatial characteristics of a ward. The variables SDPH, WLPO, LNRT, and TSRT were averaged to derive the aggregated variable ‘staff activities’ (STAC). Because the two variables involved are of nominal and interval scales respectively, Point Biserial Correlation analysis tool was used to test for this association. Results of the analysis gave an output correlation coefficient of -.033 with a significance probability point of 0.668 (p>0.05). These values, given the available data, indicate a negative, very weak and non-significant relationship between the two variables, thus, accepting the null hypothesis. Hypothesis 1 therefore states that there is no significant relationship between type of ward layout and staff activities of healthcare delivery in the study area (See Table 6). Table 6: Relationship between type of ward layout and staff activities
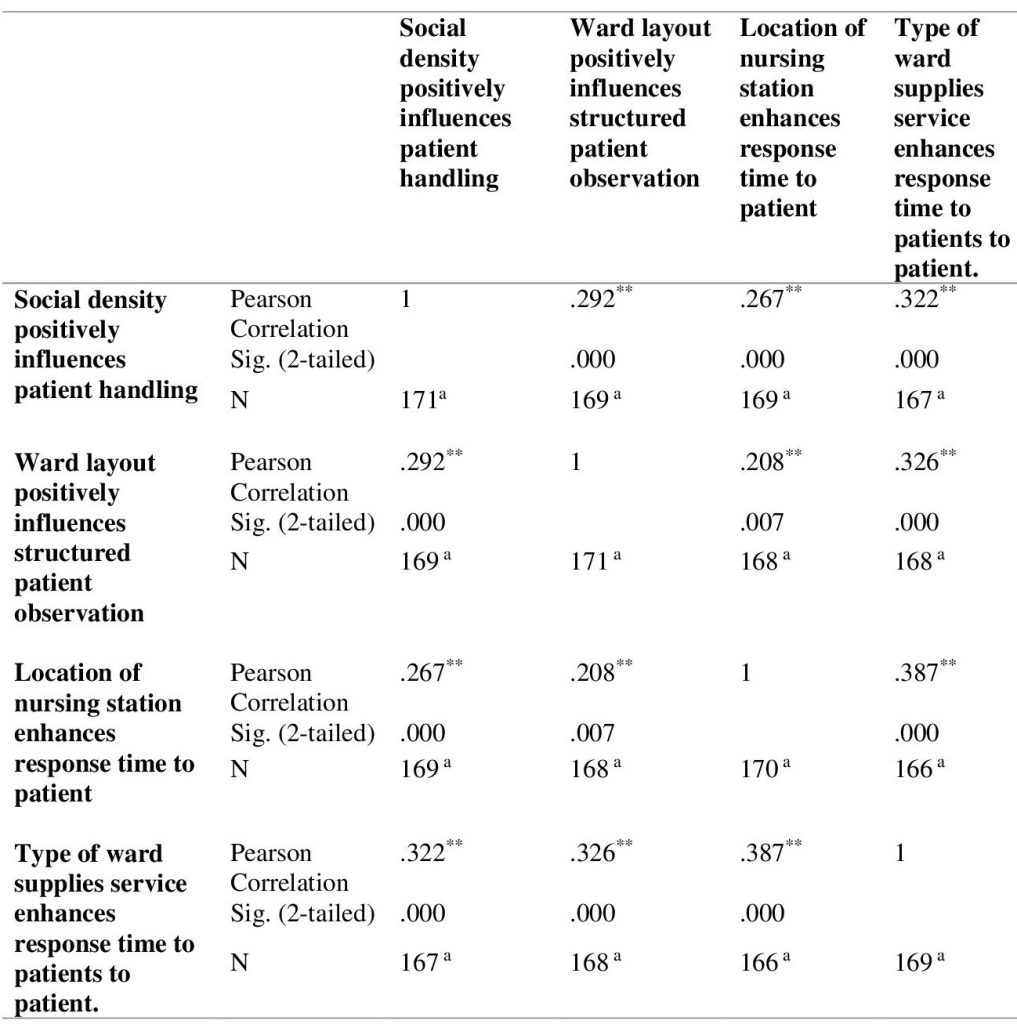
Table 7 shows the relationships between the influence of identified ward spatial features as reported by the participants. Table 7: Relationships between the influence of ward spatial features
**Correlation is significant at the 0.01 level (2-tailed). aFigures do not add up to 173 due to missing data. DISCUSSION This cross-sectional study was conducted among staff of public tertiary health facilities in Southeast Nigeria to ascertain their perception of safety as derived from the nursing station from which they operate. Respondents were drawn from MHC workers who make ward contact with patients. More than three-quarters of the responders in this study were females (77.1%). This imbalance aligns with previous studies on staffing rations in hospital settings (Alhassan & Poku, 2018; Olabisi et al., 2020; Olashore et al., 2018), and supports the conclusion that females form a greater percentage (over 70%) of healthcare and social workforce in 104 countries, including African countries (Tommasi, n.d.). The group of mental healthcare workers with less than 3 years of experience was the most common (30.8%), whereas personnel with over 9 years of experience made up only 11% of the sample. This finding is consistent with a study conducted in Botswana, where staff with 4 years of experience or less formed the majority of respondents at 50.6% (Olashore et al., 2018). Similarly, in a comparable study, Olabisi et al. (2020) found that the least experienced group of workers was the most prevalent (>6 years, 28.2%). While the difference in value labels of the variable of interest in studies may explain this disparity, a commonality can be inferred from these findings. Specifically, in specialist and teaching hospitals, residents and interns typically have 3 years of experience or less and are assigned everyday duties of healthcare delivery on the ward under the supervision of consultants and registrars. The study found that nurses constituted the highest proportion of respondents (60.1%) compared to other healthcare personnel, a finding that is consistent with several studies across healthcare settings (Haines, 2017; Kwobah et al., 2023; Olashore et al., 2018; Ukpong, 2011). Given their frontline position in providing patient care, nurses are likely to interact most frequently with the physical environment of the ward in the cause of healthcare delivery. A study by Sajadi et al. (2019) found that nurses were the most frequently encountered staff members by patients in psychiatric hospital settings. The study also indicated that patients had more positive interactions with nurses compared to other staff members, suggesting that nurses have a significant impact on patient experiences in mental healthcare settings. The question guiding the study is, ‘What is the relationship between spatial features of wards and staff activities?’ The hypothesis posited to answer this question was tested using ‘type of ward layout’ TWL and the aggregated variable ‘staff activities’ STAC (SDPH + WLPO + LNRT + TSRT). Results at a 95% confidence level gave a negative non-significant result, thus accepting the null hypothesis (r = -0.033, p=0.668). Thus, within the study area, even though open ward layouts negatively correlate with overall staff activities, there is insufficient evidence to support this. The relationship between affordances of specific physical characteristics that may influence staff activities was examined. These are: ‘influence of ward layout on patient observation WLPO’ and ‘influence of location of nursing station on response time to patients LNRT’. A significant positive correlation was outputted, implying that an increase in WLPO results in an increase in LNRT. Thus, improved patient observation as a result of type of ward layout enhances how quickly a staff responds to a patient in the event of planned or reactive patient contact. These findings align with those of Yi (2010) and Yi and Seo (2012) who assert that increased visibility of patients in the ward allows for more direct observation, thereby improving response time to patients. CONCLUSION AND RECOMMENDATION The physical environment in which healthcare delivery is executed, undoubtedly, plays an important role in staff activities of direct patient care. Other factors staff competencies, organizational culture and service process design also influence user and organizational outcomes (Ulrich et al., 2010). As has been observed from this study, and unfortunately so, the principal drive in healthcare facility design (or conversion-of-use of already existing buildings for healthcare purposes) has been the provision of spaces to execute hospital functions rather than the creation of healthcare environments that are psychologically supportive mental healthcare provision. Consequently, the study has substantiated, based on available data from the sampled facilities, the significant relationship or absence thereof, of specific physical ward features and targeted aspects of staff activities within the study area. While all the relationships between the influences of these ward features were positive and significant, certain ward features did not significantly correlate with overall staff activities, such as type of ward layout and social density. These findings, though inconsistent with previous studies, may be influenced by the differing socio-cultural context within which the study was carried out. Thus, even among healthcare providers, there is gross contempt for and lack of empathy towards the mentally ill even in the course of taking care of them, hence their responses (Chikaodiri, 2009). This ill-conceived notion thus prevents the staff from fully appreciating the affordance of the physical environment in a patient-centred mode of mental healthcare. The study therefore recommends the use of more private rooms and cubicle wards for patients with decentralized nursing stations to truly enhance staff activities, while not downplaying patient privacy. Again, there is an urgent need for healthcare providers to be trained on patient-centred model of care. COMPETING INTERESTS The author declares no potential conflicts of interest with respect to the research, authorship, and publication of this article, which is part of a wider investigation involving mental health inpatients and staff. FUNDING The author received no financial support for the research, authorship, or publication of this article. REFERENCES Alhassan, R.K. & Poku, K.A. (2018). Experiences of Frontline Nursing Staff on Workplace Safety and Occupational Health Hazards in Two Psychiatric Hospitals in Ghana. Occup Med Health Aff 6:274. DOI: 10.4172/2329-6879.1000274 Bressington, M. M., Mui, J., Hulbert, S., Cheung, E. F. C., &Gray, R. (2019). The effect of ward design on the behaviour of psychiatric inpatients: A systematic review. International Journal of Nursing Studies, 89, 80-89. https://doi.org/10.1016/j.ijnurstu.2018.09.016 Chikaodiri, A.N. (2009). Attitude of health workers to the care of psychiatric patients. Ann Gen Psychiatry 8(19) https://doi.org/10.1186/1744-859X-8-19 Gadbois, C., Bourgeois, P., Goeh-Akue-Gad, M.M, et al. (1992). Hospital design and the temporal and spatial organization of nursing activity. Work Stress: 6(3):277–91. Grootens-Wiegers, P., Heineman, E., Visch, V. T., van der Weijden, T., & de Bont, P. A. J. M. (2018). The impact of a new psychiatric hospital on patient outcomes: Before-and-after observational study. Journal of Medical Internet Research, 20(7), e10056. https://doi.org/10.2196/10056 Gureje, O. &Alem, A. (2000). A. Mental health policy Mental health policy developments in Africa. developments in Africa. Bulletin of the World Health Organization, 78, 475^482. Gureje, O., Lasebikan, V. O., Ephraim-Oluwanuga, O., Olley, B. O., & Kola, L. (2005). Community study of knowledge of and attitude to mental illness in Nigeria. The British journal of psychiatry: the journal of mental science, 186, 436–441. https://doi.org/10.1192/bjp.186.5.436 Holohan, C. J., &Saegert, S. (1973). The environment of the psychiatric ward: Problems and suggestions for research. Journal of Health and Social Behavior, 14(4), 305-316. https://doi.org/10.2307/2136919 Lauder, W., Reynolds, W., Angus, N., & Sharkey, S. (2006). Therapeutic activities in psychiatric wards: A descriptive study. Journal of Clinical Nursing, 15(10), 1267-1275 Lockman, J. C., Fisher, W. A., Hirsch, P. D., & Martinez, A. M. (2017). The impact of a psychiatric intensive care unit on the use of restraints and seclusion in an acute psychiatric hospital. Psychiatric Services, 68(6), 617-623. https://doi.org/10.1176/appi.ps.201600289 Obeidat, B., Younis, M. B., & Al-Shlool, E. (2022). Investigations into the impact of nursing unit layout on critical care nurses. Heliyon, 8(2), e08929. https://doi.org/10.1016/j.heliyon.2022.e08929 Olabisi, O., Lawal, A., Ajao, O., Adeolu, E. & Oluwamuyiwa, O. (2020). Experience and Attitude of Psychiatric Nurses Toward Inpatient Aggression in a Nigerian Psychiatric Hospital. 12. 1547. Olashore, A.A., Akanni, O.O. & Ogundipe, R.M. (2018). Physical violence against health staff by mentally ill patients at a psychiatric hospital in Botswana. BMC Health Serv Res 18, 362. https://doi.org/10.1186/s12913-018-3187-6 Reiling, J., Hughes, R.G., Murphy, M.R. (2008). The Impact of Facility Design on Patient Safety. In: Hughes, R.G. (editor). Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US): Chapter 28. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2633/ Sajadi, H. S., Mehrabian, F., & Ghaemian, A. (2019). Patients’ perceptions of mental health services in Iran: A qualitative study. International journal of mental health systems, 13(1), 1-9 Stolz, D. L., Schick, M., & Bartholomew, T. (2015). The impact of single-occupancy versus multiple-occupancy rooms on patient outcomes in psychiatric inpatient units. Journal of Psychosocial Nursing and Mental Health Services, 53(11), 28-34. https://doi.org/10.3928/02793695-20150925-03 Stuart, H., Sartorius, N., Liinamaa, T., &Levack, W. (2016). Images of psychiatry and psychiatrists. Acta Psychiatrica Scandinavica, 134(s443), 1-10. Thornicroft, G., Chatterji, S., Evans-Lacko, S., Gruber, M., Sampson, N., Aguilar-Gaxiola, S., Al-Hamzawi, A., Alonso, J., Andrade, L., Borges, G., Bruffaerts, R., Bunting, B., de Almeida, J. M., Florescu, S., de Girolamo, G., Gureje, O., Haro, J. M., He, Y., Hinkov, H., Karam, E., … Kessler, R. C. (2017). Undertreatment of people with major depressive disorder in 21 countries. The British journal of psychiatry: the journal of mental science, 210(2), 119–124. https://doi.org/10.1192/bjp.bp.116.188078 Tommasi, V. (n.d.). Value gender and equity in the global health workforce. Retrieved from World Health Organization: https://www.who.int/activities/ value-gender-and-equity-in-the-global-health-workforce. Tyson, G. A., Lambert, G., & Beattie, L. (2002). The impact of ward design on the behaviour, occupational satisfaction and well-being of psychiatric nurses. International journal of mental health nursing, 11(2), 94–102. https://doi.org/10.1046/j.1440-0979.2002.00232.x Ulrich, R.S. (2006). Evidence-based health-care architecture. The Lancet, 36(B), pp. 538-9. Ulrich, R.S., Berry, L.L. Quan, X. Parish, J.T. (2010). A conceptual framework for the domain of evidence-based design. Health Environment Research and Design Journal. 4, 95–114. Ulrich, R. S., Zimring C., Joseph, A, Quan, X., & R. Choudhary. (2004). The role of the physical environment in the hospital of the 21st century: A once-in-a-lifetime opportunity. Center for Health Design: Concord, CA. Ulrich, M. C., Zimring, C., Zhu, X., DuBose, J. R., Seo, H., Choi, Y. S., & Joseph, A. (2014). The impact of environmental design on patient outcomes in acute psychiatric inpatient units: A systematic review. Journal of Hospital Administration, 3(4), 107-115. https://doi.org/10.5430/jha.v3n4p107 |
||||||||||||||
|
||||||||||||||